IN ALBERTA, CANADA TOO – DESPERATE LIFE-SAVING NALOXONE CAMPAIGNS REDUCE HARM FROM THE LETHAL FAILURE OF OPIOID CRISIS EXPERT TREATMENTS
Even dramatic opioid death reductions from naloxone campaigns can’t stem lethal failures of “game-changing” injectable Sublocade, other expert gold standard treatments
by Clark Miller
Published January 30, 2026
The news from Edmonton, Alberta –
There were more opioid-related deaths in March than in any previous month on record in the Edmonton zone, according to the latest government data.
Two experts say more should have been done in the lead-up to the spike in fatalities.
Eighty-seven people died of opioid drug poisoning in March, making that the highest amount of opioid-related deaths in Alberta’s capital region since authorities began tracking it publicly in 2016.
“It’s very horrific, frankly, to see such a big spike in deaths in Edmonton,” said Elaine Hyshka, Canada Research Chair in Health Systems Innovation at the University of Alberta School of Public Health.
“We’re almost 10 years into this crisis. And so the fact that the numbers here are getting a lot higher, it’s really troubling.”
Those trends and concerns are for 2025.
That’s part of the story. Here’s more –
The source reasons for those systematically underestimated death estimates are reported here, in a CBC news report.
And there’s more, importantly, to the story.
From a January 10, 2026 news piece in the Edmonton Journal –
Opioid-related deaths are trending down across Alberta, but emergency room visits and emergency medical services responses to substance-related events are nearing all-time highs.
According to Alberta’s substance use dashboard, EMS responses to opioid-related events from January to September 2025 far exceeded the totals from the previous year. The province recorded 8,116 EMS events in the first nine months of 2025, compared with 4,674 recorded during the same window in 2024.
Once the final three months of data are reported, the 2025 total may equal or exceed the record 10,205 EMS responses that was set in 2023.
Dr. Warren Thirsk, head of emergency medicine with the Alberta Medical Association and an emergency room physician at the Royal Alexandra Hospital, said the situation on the ground has not improved despite numbers showing opioid-related deaths gradually declining in Alberta.
It is important to understand what these reports and trends mean.
Differences over time and between groups in incidence of fatalities due to opioid overdose have never been valid measures of the severity or course of opioid use epidemics, because those measures have always been confounded by concurrent differences in distribution and use of naloxone (from at least as early as the 1970s) to reverse overdoses that otherwise would become fatal. Those reversals have no impact on the forces and circumstances driving users to engage in high-risk opioid use.
That is in clear and distinct contrast to medical and other forms of “treatment” that can provide benefit and moderation of epidemics only if and to the extent that they result in avoidance of high-risk opioid use with associated risk of nonfatal overdose, fatal overdose, and other harms.
Every instance of the use of naloxone to prevent an otherwise fatal overdose is, in fact, an incidence of failure of standard, expert opioid crisis “treatments”.
Those intractable facts compel us to be very intentional and thoughtful in interpreting data and evidence related to an opioid epidemic that has worsened over decades.
Unlike fatal opioid overdoses, trends and differences in nonfatal opioid overdoses have been a more valid measure of severity of the crisis, but more recently with important qualifications. Those nonfatal overdoses have, as intensive, dramatically successful naloxone campaigns have placed rescue units in the hands of laypersons in homes and communities, become gross underestimates when based, as they always are, on records of reversals from hospital visits or emergency responders, those reversals a diminishing proportion of total reversals occurring.
That is to say, in Alberta, Canada, the opioid crisis is worsening.
Worsening despite dramatically successful naloxone campaigns reducing fatal overdoses.

Naloxone campaigns in Alberta intensified pre-COVID and, most importantly, focused on getting kits into the hands of laypersons proximate to high-risk opioid users, because in an overdose, every second counts.
Those efforts resulted in “year-over-year” increases of 47% from 2020 to 2021 –
And those efforts have continued, per Dr. Warren Thirsk, head of emergency medicine with the Alberta Medical Association, in this 2026 report –
Thirsk believes there’s been more naloxone than ever distributed and health providers have been adept at responding to opioid overdoses and catching them quickly before they escalate. Shelters have also become more equipped to handle multiple overdoses, he added.
That brings us to a point at which some explanations are demanded, and explanations owed to Albertians, Canadians and Americans, to anyone who has trusted in the public health experts, institutions and media to provide truth and competent guidance to address the lethal crisis worsening over decades.
Because in Alberta, the persistently worsening crisis, moderated only by desperate, intensive naloxone campaigns to reduce the death count from increasing high-risk opioid use, has occurred over years of gold standard “treatment” expansion investment of $200 million, in a province of about 5 million Canadians.
And because the focus of that $200 M investment was provision of the “game-changing” proven, expert opioid cure Sublocade, an injectable, 30-day formulation of buprenorphine that cannot be diverted or used, like other “bupe” formulations, as street currency for fentanyl.
That investment in provision of the gold standard, injectable medical opioid cure began in 2021.
The Alberta government announced Wednesday it will fully cover the cost of the injectable opioid treatment drug Sublocade.
As opposed to tablet versions, the injectable treatment lasts in a person’s system for 30 days and provides stabilization, reduces cravings and provides enhanced protection against overdose, the province said.
“There is hope for people with addiction,” said Mike Ellis, associate minister of mental health and addictions. “Recovery is possible.”
“This option will save lives,” Ellis said.
“The addition of Sublocade to the publicly funded formulary and removal from special access will significantly reduce barriers to this medication. Recovery-oriented care is about providing options to Albertans with addiction and this option will save lives and support recovery,” Ellis added
Having the costs of Sublocade covered “will be a game-changer for addiction treatment in Alberta,” said Dr. Monty Ghosh, president of the Alberta Medical Association.
“This will increase treatment options for individuals with opioid addiction. Addiction medicine physicians across Alberta will be grateful to have another tool to treat opioid addiction, especially for our various vulnerable clients who previously could not afford this life-saving medication.” …
“That option is important to have on the table for some people who have an opioid addiction disorder,” said Elaine Hyshka, assistant professor at the University of Alberta’s school of public health. “Cost should not be an impediment to access care.
That’s high praise – and from a consensus of experts! – for a “treatment” that was, predictably, bound to be evidenced as lethally failing.
Alberta went in full tilt for Sublocade.
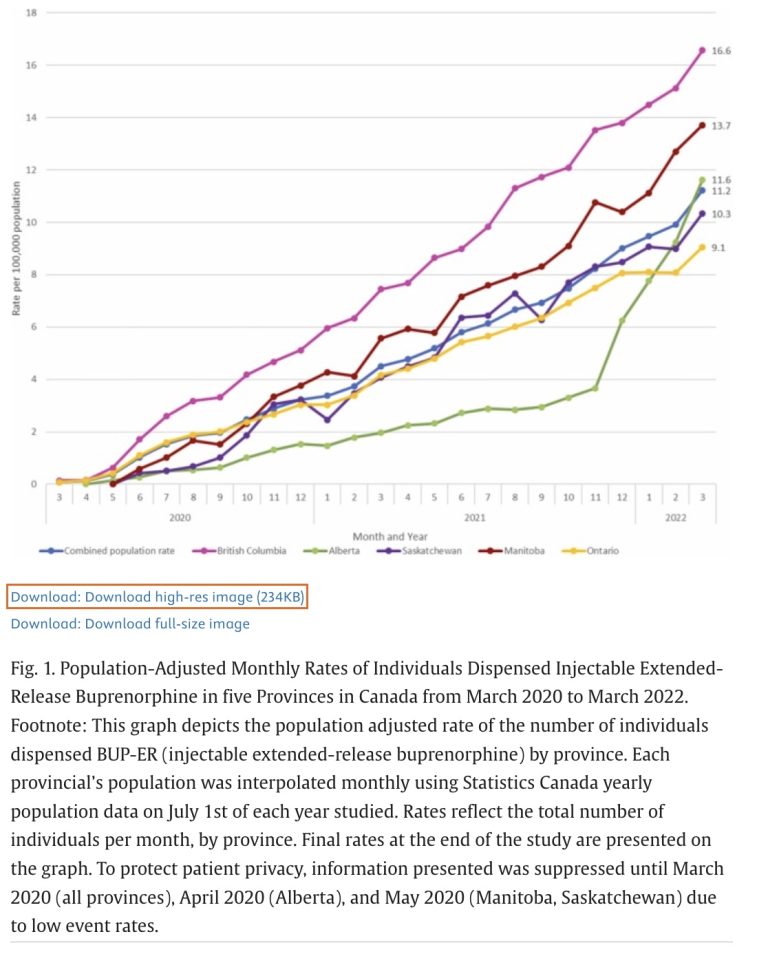
(Alberta data are represented by the green line in the first two figures below. )
Highlights
Extended-release buprenorphine (BUP-ER) is a novel form of treatment for opioid use disorder available in Canada since 2020.
Use of BUP-ER rose quickly across Canada since approval, but varied by province.
BUP-ER use is highest in rural regions, reflecting improved accessibility to treatment in some parts of Canada.
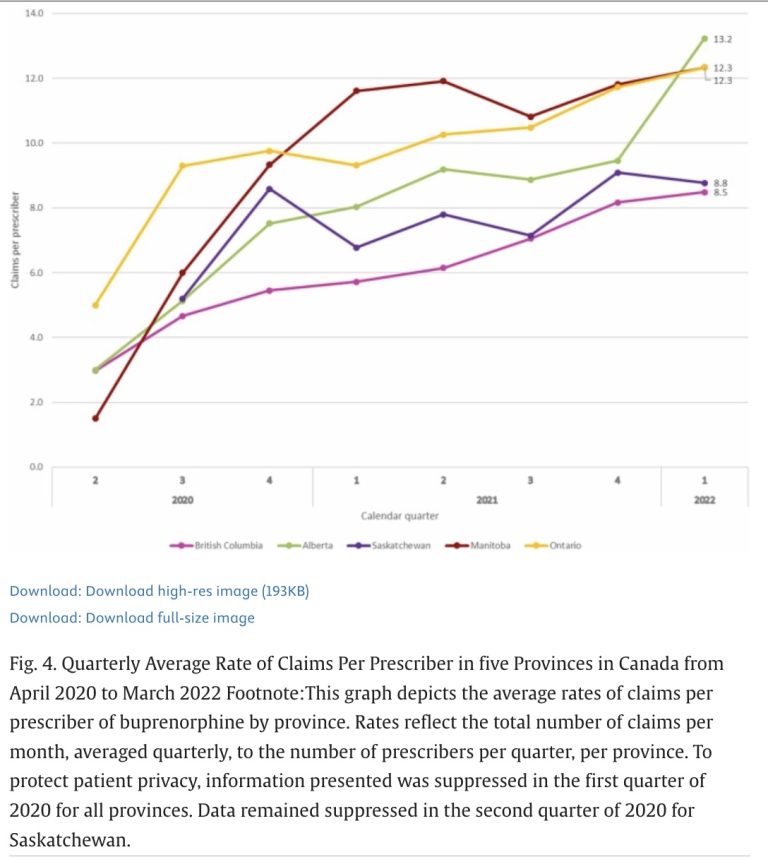
Here’s another line graph comparing Canadian provinces.
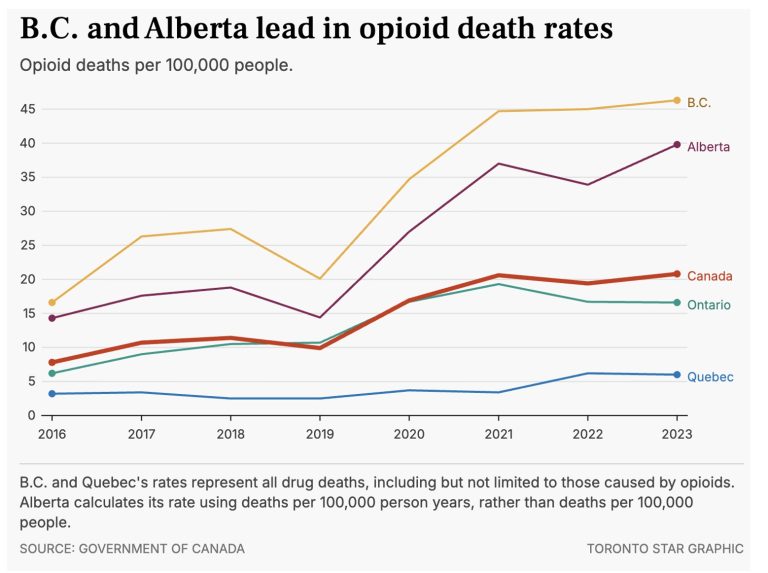
In this case, data illustrate how opioid overdose deaths surged in Alberta compared to other provinces during and immediately following the years over which the provision by medical providers of “game-changing” sublocade was surging.
From a 2021 report on Alberta’s treatment expansion –
“We’re building five new long-term drug addiction therapeutic treatment communities across the province, including partnerships with First Nations communities that have been hard hit by the opioid crisis.”
The province has put more than $200 million into initiatives to address the opioid crisis, the premier said.
And from this 2025 CBC report, traditional gold standard treatments for problem opioid use continued to expand per Nathaniel Dueck, press secretary for the Ministry of mental health and addiction –
“He said Alberta started accepting clients at three of its recovery communities starting in May 2023, with eight more being established as part of its response to the addiction crisis.
The province also said it added more than 10,000 publicly funded treatment spaces and removed daily user fees for residential treatment.”
Things just don’t add up.
Or do they?
Actually, things always add up,
just not in ways they are desperately needed to, but for anyone overcoming the cowardice that would otherwise inhibit and blind them from seeing and expressing the obvious.
Obvious, from decades of evidence, that:
There has never been strong, let alone compelling evidence (and here) that American Medicine’s gold standard cures for substance use provide benefit.
Or that substance use is a medical condition at all, treatable with medical interventions.
It turns out, as explained and established here in multiple posts, that precisely as in the avoidable – avoidable if not for the cowardice and gross incompetence of American Media – generation of the opioid crisis as we know it enabled by fabrications by America’s medical/research/media collusion, there has never, not ever, been a legitimate body of research evidence to confidently establish, let alone strongly support, the use of substitute opioids (bupe or methadone) as treatments or as beneficial for opioid dependence.
Instead, all lines of diverse evidence point to what should be obvious – the runaway dispensing of opioids that are routinely used with other, illicit opioids (methadone), and/or serve as consumable, commodity and currency in street economies of illicit high-risk opioid use (bupe) have in fact fueled the lethal epidemic.
The most potent ways in which the “miracle” doctor-dispensed pills and other magic potions predict failure is to instill in compulsive substance users the belief that passive interventions to adjust brain chemistry are “treatments”, are addressing a generic neurobiological block or deficit or disease of the brain that explains addiction, instead lethally instilling passivity, dependence and lies, and robbing compulsive substance users of the necessary factor established as central to stopping problem use, self-efficacy, the shift to belief in one’s own competence, autonomy, strength, and effective use of resources with inner psychological change to do away with the compulsion to escape distressing inner states by use of chemicals.
Some lies must be desperately protected, no matter the cost.
Related post coming up soon:
“SUBLOCADE: MORE LETHAL OPIOID CRISIS LIES – IN AMERICA’S TOP MEDICAL JOURNAL”