IN ONTARIO CANADA TOO: A WORSENING OPIOID CRISIS HIDDEN BY EMERGENCY NALOXONE SAVES
It’s the same predictable story everywhere – desperate, emergency naloxone campaigns reduce fatal opioid overdoses while lethal expert treatment failure fuels increasing high-risk use and overdose
by Clark Miller
Published January 16, 2026
What “same predictable story”?
This one, in Hamilton, Ontario in Canada, reported in the Hamilton Spectator.
At a time when paramedic calls for opioid overdoses are at an alltime high in Hamilton, the board of health passed a motion Dec. 1 to expand public health’s semiannual update on the situation. …
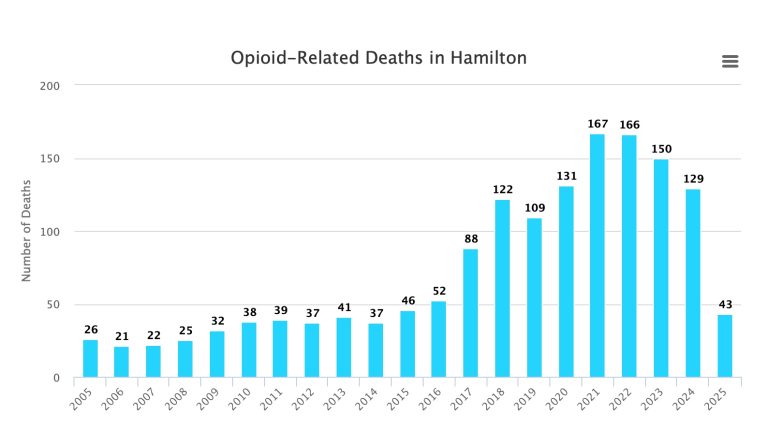
The report presented to the board showed diverging trends. On the one hand, paramedic calls for overdoses were the highest since reporting began, with 418 responses from July to September. July set a record at 134 calls — the previous high was 109 in August 2021. That July record was promptly broken, with August and September each having 142 calls.
At the same time, deaths have been going down. There were 37 confirmed or probable opioid-related deaths from January to June 2025 — the most recent data available. It is among the lowest during a six month period since 2019.
[emphasis added]
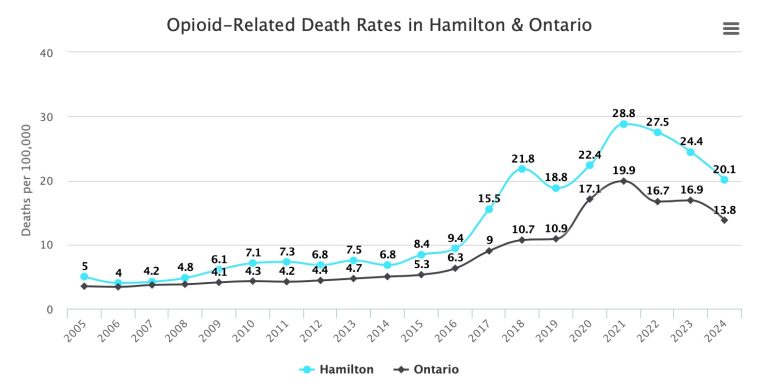
Hamilton and province Ontario following similar patterns
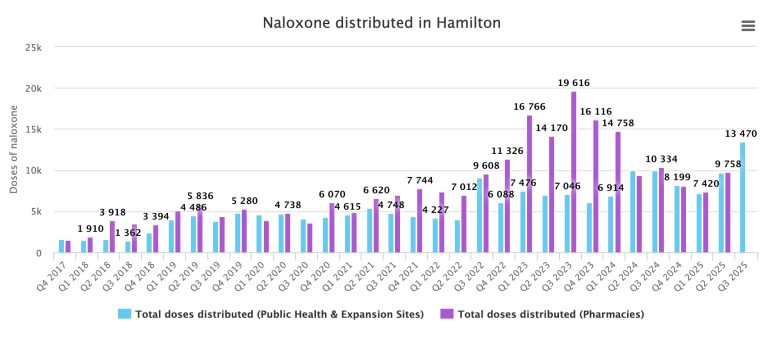
And predictably, a tight temporal correlation with public availability of naloxone, distributed for use to reverse potentially fatal opioid overdoses.
Comparing the graphics, it’s important to note –
The difference in timescale for naloxone distribution
That total naloxone distributed is the sum of each pair of differently-colored bars each quarter
That naloxone distribution was to sites (pharmacies, community programs, public health) directly providing units to laypersons (opioid users, their families, peers and friends), not law enforcement or first responders and
Naloxone distribution surged from late 2022 through 2023, remaining high thereafter, corresponding to initiation of and sustained dramatic drops in opioid deaths through 2024 and 2025
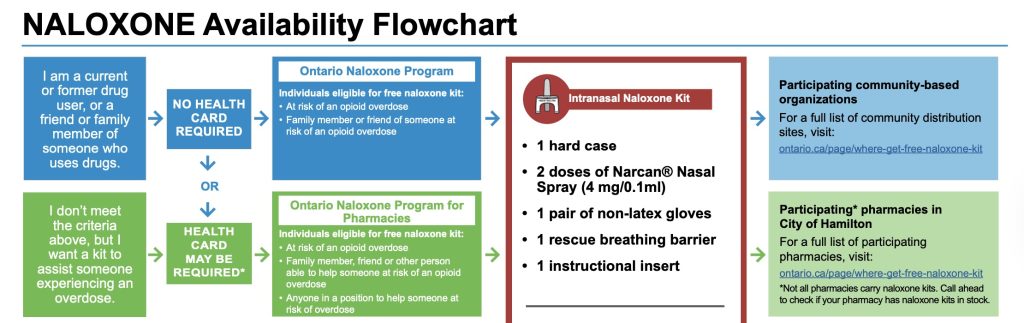
That naloxone being distributed was being effectively distributed, as established by practices and research affirming the heightened importance of getting the Narcan units in the possession of those proximate to potential overdoses, like peers, family, and friends, when every second counts.
Free take-home naloxone kits are available at select pharmacies and community agencies in Hamilton—no prescription needed.
Public Health Services partners with shelters, outreach programs, and other community agencies to distribute harm reduction supplies and naloxone. If you’re connected with a community agency and need naloxone, ask if they provide it or can help you access it.
Kits are for people at risk of an opioid overdose, their friends and family, and anyone who may need to respond to an overdose. You can pick up a kit and receive naloxone training at participating locations.
You can pick-up naloxone at any of the following locations in Hamilton, during operating hours: …
That all makes sense,
and serves as yet one more example of a locale, consistently, where the evidence further affirms what is established: that in the U.S., Canada and almost certainly elsewhere, it is desperate, emergency, effective naloxone complaigns that solely account for recent and historical drops in opioid-related deaths, not other factors.
But what about the increasing EMS calls for opioid overdose? How does that fit in? As opioid deaths are declining?
Exactly as predicted based on what is established consistently by research and congruent evidence.
As explained and supported by linked-to evidence and research repeatedly in multiple posts at A Critical Discourse –
Emergency, intensive naloxone campaigns have arisen desperately as harm reduction against a worsening crisis precisely because high-risk opioid use continues to mount.
High-risk opioid use is a direct measure of expert gold standard treatment lethal failure, those “treatments” beneficial only to the extent that they prevent high-risk use.
America’s expert gold standard “treatments” that have been lethally failing over past decades while substance use epidemics worsen are not treatments at all, instead represent individual and institutional pathological levels of research illiteracy, delayed ethical development, reckless ignorance, and impaired capacity for critical thought. There are no “game changers” within systems that sick.
And those naloxone saves?
The only moderating factor to reduce harm predicted by expert treatments in a worsening opioid crisis?
That’s a dead end.