MISINFORMATION SERVES LIES THAT PROTECT LETHAL HEALTHCARE PRACTICES: MICHIGAN OPIOID CRISIS OUTCOMES
Desperate, effective naloxone campaigns in Michigan saved lives, those community-based outcomes spun by state experts to hide a worsening epidemic
by Clark Miller
Published November 7, 2025
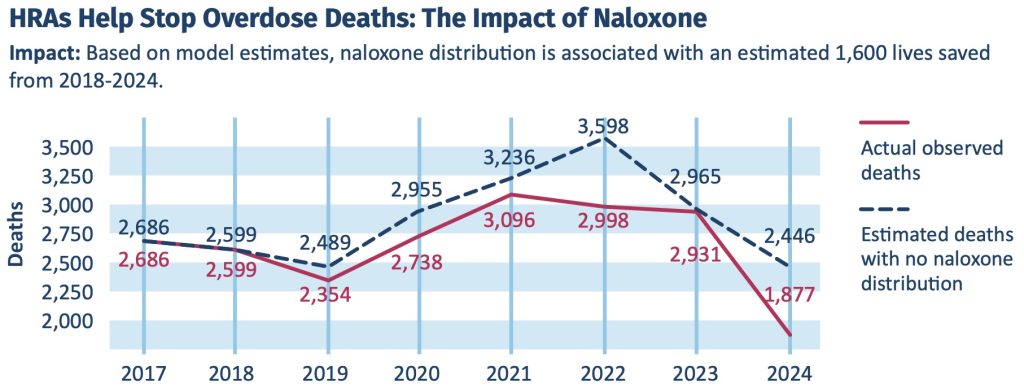
At first glance, the 3-page report from the Michigan Department of Health & Human Services (MDHHS) appears grossly accurate and promising. The role of intensive, successful life-saving naloxone campaigns in Michigan (here and here) is highlighted, aptly, as those saves have more than accounted for all reductions in opioid overdose deaths over recent years.
And let’s be clear, those naloxone campaigns that have so successfully reversed upwardly surging fatal opioid overdose trends have been desperately necessary and ethically unassailable, with full benefit undetermined.
And that, as we’ll see, is far from the whole story, which will require second, third, and multiple looks at the data as presented and at the conveyed portrayal of gains against a worsening crisis.
Although it’s clear from reading between the lines, and by the prominence in the report of naloxone (its role solely in reversing a potentially fatal opioid overdose), it’s hard to find the words “opioid” or “opioids” in the report, and a disclaimer or two warn against drawing causal inferences from the data presented graphically or otherwise. As we’ll soon see, providing that advisory – that the meaning of the data and trends may be entirely different than represented – was sound judgment.
But in media reports and statements from public health professionals involved, there is no indication that the evidence could be pointing in any direction other than public health experts and institutions making gains against the epidemic.
From this report in the Huron Daily Tribune.
A new Michigan study is showing changes in the number of people dying from opioid overdoses and the branching positive impacts from harm reduction services. …
Elizabeth Hertel, Michigan Department of Health and Human Services director, said in the release that Michigan ranked in the top five states “for greatest reduction in overdose deaths.”
“Harm reduction is a key component of our opioids response in Michigan, and it is working,” Hertel said.
“our opioids response … is working”
Let’s break this report down.
The Devil, some say, is in the cowardly media accounts and spun messaging of self-preserving, dysfunctional systems of power, so it may be worth taking a look.
But first, a preview.
From what we know about the course and causes of America’s worsening opioid crisis,
and from 3 previous posts at ACD on Michigan’s response to it (here, and here, and here) –
– It is established that the widespread, intensive, community-based, targeted, successful naloxone campaigns over past years have accounted for all – more than all – of recent-year drops in fatal opioid overdoses.
– Those drops are not explained by other factors, ruled out after being generated to attempt to mystify what is clear –
– that the desperate, intensive campaigns of emergency naloxone reversals are necessary precisely as harm reduction due to lethal failure of American expert, gold standard treatments.
– The very success of those campaigns, depending on shifting naloxone reversals – when every second counts – to street, layperson, and community settings has had the addiitonal effects, due to underreporting of Narcan reversals = nonfatal opioid overdoses, of underrepresenting nonfatal opioid overdoses = high-risk opioid use = gold standard treatment failure.
Back to the report –
HRA = harm reduction agency
Okay, so the surges in naloxone saves (prevention of potentially fatal opioid overdoses) over recent years in Michigan resulted in fewer opioid OD deaths. That is incontrovertible. But the rest of what is conveyed by the graphic is a lie, a lethal lie.
That’s because we know that increasingly over those years represented, saves were occurring in community, layperson settings and were not reported. Not incorporated into any medical record that could be searched and used in research reports. Yet as real as any reversals and often reported to the direct-service community providers “on the ground” implementing the successful naloxone campaigns.
We don’t know the source for MDHHS for opioid potentially fatal ODs reversed by Narcan, but can be very confident based on all other formal accounting provided publicly – that it was by use of accessible medical databases, generated by emergency responder, emergency department, or hospital records.
To repeat: it’s established that over recent years of shifts to layperson, community-based use of Narcan to reverse potentially fatal overdoses, increasingly those nonfatal overdoses are going unreported and unaccounted for, not becoming part of medical or other databases.
So, let’s compare the estimate noted in this post from community direct service providers to what MDHHS provides in the graphic provided to us. From the most recent psot at ACD on Michigan’s response to the opioid crisis –
From this recent post, estimates of reversals by a single organization involved in Narcan distribution included 6,600 over the period 2020 to 2023, and 2,600 potential OD deaths reversed in fiscal year 2023 (October 1 2022 to end of September 2023).
Even if adjusted by a factor of 0.1 downward to account for multiple administrations and other errors, those numbers more than account for the modest declines in fatal opioid ODs over those periods. And the reported “nearly 34,000 reported uses to reverse overdoses and save lives” adjusted to 3,400 is also many more than needed to account for recent drops in opioid OD deaths including in 2024.
That is, after the effects of naloxone reversals – directly witnessed and reported – there simply are no remaining reduced fatal overdoses to account for.
But let’s take a closer look at the evidence. After all, attributions of reduced deaths to various other factors have come from recognized experts and authorities.
Back to our current post –
So, a single agency in Michigan involved in harm reduction, including the distribution of naloxone kits, based on reports to them estimated use of naloxone to prevent potentially fatal opioid overdoses over fiscal 2023 as 2,600.
From the graphic in the MDHHS report, there were an estimated 30 – 40 opioid OD deaths prevented by naloxone over 2023.
The discrepancy is stark, yet predictable considering the known shifts in reversals from involving medical services and being incorporated in the types of medical or insurance claim databases used to research these trends, to being reported to the direct service agencies providing the distribution and re-supply of Narcan kits, but not incorporated in any such database.
The takeaway, of course, is that to the extent that we adjust our interpretations to reality- and evidence-based, the trajectory of projected opioid overdose deaths without the intervention of naloxone would be seen increasing, actually skyrocketing, representing persistently increasing high-risk opioid use and potentially fatal overdose.
Next
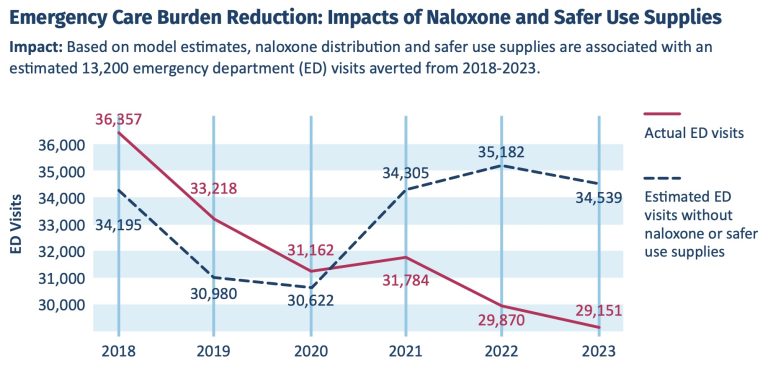
“Fewer Hospitalizations Reflect Harm Reduction in Action”
Yes, maybe, but predicting harm and hiding the severity of a worsening crisis. Let’s consider.
And let’s fix that graphic title: “Fewer Hospitalizations Reflect Dramatic Shift to Layperson Naloxone Reversals with Avoidance of Medical Attention”

Let’s consider starting with the vague and careful language used to describe this graphic:
Based on model estimates, without harm reduction efforts, Michigan may have seen more than 13,000 hospitalizations related to injection drug use between 2018-2024.
The “model” is a mystery, as are sources of data for the model, so emphasis on “may have”, and it seems important to note that – based on real data rather than projections – hospitalizations increased from 2023 to 2024.
But there is a far more important consideration here, one that returns us to the established trend of recent-year dramatic, community-based naloxone campaigns resulting in life-saving Narcan reversals occurring more and more frequently by laypersons, with no emergency or other medical involvement, and remaining largely undercounted.
There are, of course, a variety of powerful incentives for many or most high-risk opioid users to avoid medical attention and a near-fatal overdose becoming part of a searchable record, once revived by peers or others in the community.
But that fast, proximate peer or layperson response that saved a life and avoided medical (and other) attention has costs. There is no one involved in that type of response who might otherwise identify over the course of an ED visit and gain consent for a hospital admit when an overdoser presents with any of a variety of injection drug-related conditions that would advise hospitalization. That is, the naloxone campaign DIY revolution, while moderating OD deaths tied to gold standard treatment failure, has the unintended effect of hiding from view the health costs and legitimate, missed need for hospitalization for conditions associated with high-risk opioid use and a persistently worsening crisis.
Maybe that’s why mobile units addressing wound care and other medical needs are increasingly noted in news reports. And maybe that fits with, for example, the observations of one direct service provider in Vermont –
Tracie Hauck, executive director of the drug recovery group Turning Point Center of Rutland, said focusing on death data alone could be misleading.
“From what I see in our community, things aren’t any better,” she said. “Crime is picking up again. You’re seeing people that are struggling health wise and have no place to live and are using substances.”
Whatever the above graphic “may” convey as intended, what we know it does reflect is that the shift to disaster medical response, to mobile, street medicine replacing hospitalization as needed, is not a good thing, hiding the costs of a worsening epidemic.
And what about opioid-related emergency department (ED) visits?
The same established facts, trends, and considerations apply here as were covered above.
Across the country, ED visits and emergency medical response (EMR) for opioid overdoses are trending down, clearly and necessarily tied to the associated trend of dramatic shifts in potentially fatal opioid ODs being reversed “on the street”, in community settings, by laypersons and with high-risk opioid users declining medical attention once revived.
Those trends, of course, do not represent a moderation of high-risk opioid use or overdose, instead hide what is established as a worsening course.
Opioid injection-related infectious disease is a valid measure of high-risk use and severity of the crisis.
But, as always, meaningful interpretation of the data and trends requires critical thought.
For a decreasing trend of incidence or prevalence of an injection-related infectious disease, multiple factors may be causative, including, for example, higher rates of detection and treatment, successful public health prevention gains unrelated to injection drug use, or gains in reduction of injection-related transmission by reduction of high-risk opioid use.
Note that the model estimates for this graphic combine effects of “Medicaid initiatives to treat people living with hepatitis C virus (HCV)”, predicted to significantly reduce cases. As far as can be discerned from the model and graphic, all of the apparent reductions in cases are attributable to medical treatment and none to effects related to injection drug use.
It’s a different situation when rates of injection-related infectious disease are increasing, as they have been over past years and decades. That’s because potentially we should be able with relatively high confidence to rule in or out possible confounding factors for that type of increase related to changes in public health, prevention, or treatment.
But more to the point. In this graphic and those preceding, Michigan state health officials have only confused and obfuscated vitally important questions about the course of a decades-long, persistently worsening opioid crisis and the desperate need for new direction in addressing it.
To the extent that the deceptive distortions convey a message of gains against that crisis, they constitute lethal medical misinformation.
What we know, to repeat points we began with:
– It is established that the widespread, intensive, community-based, targeted, successful naloxone campaigns over past years have accounted for all – more than all – of recent-year drops in fatal opioid overdoses.
– Those drops are not explained by other factors, ruled out after being generated to attempt to mystify what is clear –
– that the desperate, intensive campaigns of emergency naloxone reversals are necessary precisely as harm reduction due to lethal failure of American expert, gold standard treatments.
– The very success of those campaigns, depending on shifting naloxone reversals – when every second counts – to street, layperson, and community settings has had the additional effects, due to underreporting of Narcan reversals = nonfatal opioid overdoses, of underrepresenting nonfatal opioid overdoses = high-risk opioid use = gold standard treatment failure.
And more than that, we know that the signs of a worsening crisis in Michigan (here and here and here), despite efforts to conceal them, are consistent with all other valid measures of severity and worsening course of the epidemic, including nonfatal overdose, incidence of opioid injection-related infectious disease, workplace random drug screens, and the necessity of desperate, intensive naloxone campaigns as harm reduction against failed, lethal gold standard medical treatment.
What is emerging is that reliance on emergency overdose reversals is not sustainable, is a dead end.
That’s covered here, in this recent post, and in the upcoming post, “THE LETHALLY LAID NARCAN TRAP”.